UP-PGH Department of Dermatology: 100 Years of Skin Health Advocacy in the Service of the Filipino. Is there a place for the dermatologist in primary health care?
DOI:
https://doi.org/10.47895/amp.v58i17.11680Abstract
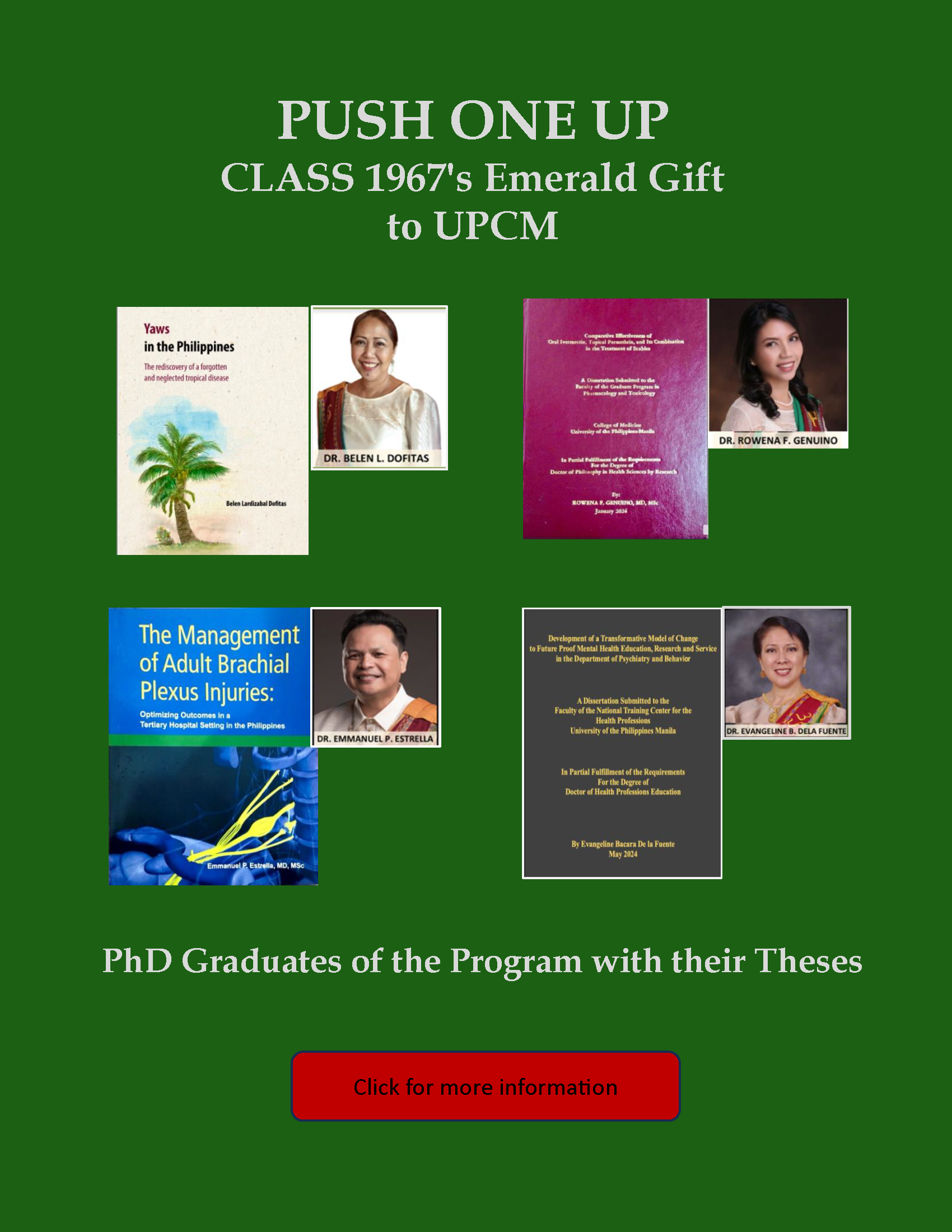
The Department of Dermatology of the University of the Philippines – Philippine General Hospital has celebrated its 100th year last 2022. Recognizing the importance of skin health, the Division of Dermatology was established in 1922, merely 12 years after the Philippine General Hospital was formally inaugurated and had opened its doors to the public. It is notable that among the researches of its first chief, Dr. Perpetuo Gutierrez, also considered The Father of Philippine Dermatology, were on yaws. Yaws, a bacterial skin infection caused by Treponema pallidum subspecies pertenue, was considered as one of the most important public health problems in the Philippines in the mid-twentieth century. It was thought to have been eradicated in the Philippines since 1973, after a nationwide yaws eradication campaign was initiated in the 1950s. However, Dr. Belen Dofitas, chief of the Department’s Section of Neglected Tropical Diseases, had detected yaws cases in Mindanao in 2000, alerting the DOH that yaws is still endemic in certain populations. In fact, one of the goals of the 2024 DOH’s Multi-Disease Elimination Plan includes stopping the transmission of yaws. Then and now, UP-PGH Department of Dermatology has been blazing the trail towards skin care for all Filipinos.
With the signing of the Universal Health Care (UHC) Bill into law, what is in store for dermatology in the Philippines? At present, patients with skin concerns are able to consult dermatologists directly, without any need for a referral from a primary care physician. With the UHC law, dermatologists being considered specialists may only be consulted by patients upon referral from the health system’s gatekeepers, the primary care physicians. Specialists may still be consulted directly but at a cost. This model is not new, and has been the set-up followed in developed countries such as the US, UK, and Canada. With the aim of providing quality health care, the goal is to move the health system’s focus from treatment to prevention. The vision is for every Filipino to have access to a primary care physician, as well as all preventive care and counsel near one’s residence. This goal will not be achieved overnight, and requires constant education in health literacy, not just for patients, but also for physicians and everyone in the health system. Primary care physicians will therefore be expected to provide high quality health care in all aspects. It is worthwhile to consider if this is truly feasible in this age of information explosion and therapeutic innovations. Will this path really lead to better patient care open to innovations, or just health insurance-directed care?
This system has its pros and cons. There are anecdotal stories from countries following this system, of long waiting times before patients are seen by primary care physicians, and more so by specialists, including dermatologists. Dermatologists are trained to see any patient with any skin concern, from common dermatoses such as acne, tinea, impetigo, and pediculosis, to less common and relatively more complicated cases such as autoimmune bullous diseases and skin cancer. At the PGH Dermatology OPD clinic, the top ten diseases based on new patients in 2023 were 1) acne vulgaris, 2) psoriasis, 3) keloid, 4) atopic dermatitis, 5) irritant contact dermatitis, 6) melasma, 7) verruca vulgaris, 8) seborrheic dermatitis, 9) dermatosis papulose nigra, and 10) nummular dermatitis. The cumulative census of all residency training institutions of the Philippine Dermatological Society (PDS) last 2023 based on new cases reflects a similar trend: 1) acne vulgaris, 2) scabies, 3) dermatophytosis, 4) psoriasis, 5) seborrheic dermatitis, 6) atopic dermatitis, 7) allergic contact dermatitis, 8) verruca vulgaris, 9) irritant contact dermatitis, and 10) lichen simplex chronicus. These also make up the cases seen by most dermatologists engaged in private medical practice. Although these cases may be seen and managed with competence by primary care physicians, these are cases which dermatologists have been trained to manage, educate, and spend time providing counsel. The gatekeeper model will not be cost-effective if patients with skin conditions will ultimately be referred to dermatologists after being seen by primary care physicians. This model may be more appropriate for patients who have vague symptoms and do not know which physician to consult. However, patients with skin symptoms do have skin diseases and may choose to consult a dermatologist.
As the Universal Health Care Law is still in the process of full implementation, it is timely to consider if it is better that dermatologists as well as other specialists that focus on certain organ systems such as ophthalmologists, otolaryngologists, and orthopedic surgeons, be offered the option to be embedded in primary health care. This will allow patients to directly access their expertise, with shortened waiting times and be assured of quality care. This will also lessen the patient load of primary care physicians who will continue to see a variety of patients, allowing them to provide better health care to all their patients.

.jpg)